Please join the OptiBreech Collaborative fetal monitoring case review seminar on Wednesday, 22 February, 8.30-9.30 – via Zoom.
Revised flowchart for decision-making in the second stage of breech births – revised Algorithm. The OptiBreech Collaborative welcomes your thoughts on this new version.
Permission given to share this post and video freely with anyone who may find it helpful, including women in your care or colleagues.
Transcript
Hello. My name is Shawn Walker. I’m a Consultant Midwife, the Clinical Lead and the Chief Investigator of the OptiBreech Trial.
In this video, I am going to speak directly to women who may be planning a vaginal breech birth under OptiBreech care, but the information is also to inform the healthcare professionals who may be caring for you.
Within the OptiBreech Trial, we have observed an increase in complications among births where either meconium-stained amniotic fluid or fetal tachycardia are observed during labour, and especially when they are both present. I’m going to explain each of these things in turn so that you understand exactly what we are looking for and why our OptiBreech teams will be giving you advice they give you if they occur during your birth.
Meconium
First, meconium. Meconium is the baby’s first poo. When it first comes out, it looks like thick black tar. In a textbook, ideal vaginal breech birth, where the baby has coped beautifully in labour, this black tar substance first emerges around the same time we begin to see the place it emerges from! At this point, your baby is being tightly hugged in the final few moments before they are born, and it basically gets squeezed out of them like a tube of toothpaste. We’re fond of calling it ‘toothpaste meconium.’ This is completely, 100% normal and will occur in every breech birth.
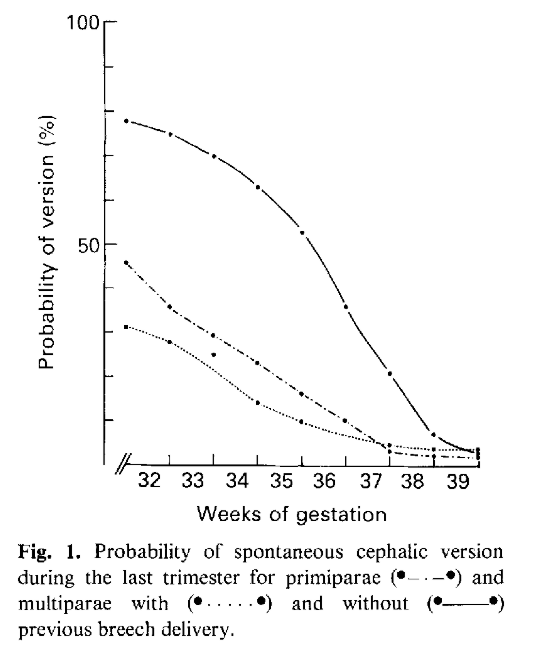
However, when babies pass meconium before they are born, that’s a bit less straightforward. The meconium mixes with the fluid around your baby, the amniotic fluid. Professionals call this, meconium-stained amniotic fluid. It’s a fairly common occurrence. We see meconium in about one out of seven pregnancies. Occasionally, babies pass meconium when they are still inside after 40 weeks of pregnancy, or past their expected date of birth. Their bowels are more mature and ready to get moving, so they do. Sometimes it doesn’t mean anything more than a bit of extra mess.
But sometimes, passing meconium during labour is a sign that baby is finding it a bit stressful. Again, most of the time, babies can handle a little bit of stress in labour, just like their mothers. But if meconium is identified early in labour, we have advised our OptiBreech teams to err on the side of caution and offer you a caesarean birth. This is because we have observed that when we see meconium early in labour, we observe additional complications later in labour more often. There still may be a long way to go, and most women tell us they would prefer to avoid a rushed, emergency caesarean birth late in labour. The earlier we do a caesarean if it looks like it may be necessary, the more calm and relaxed everyone can be, and the safer it is for you and your baby.
So we want to offer you the information that there is some increased risk of this happening if meconium is present early in labour. But of course, this decision is always up to you. You may want to ask your OptiBreech team for more information about other signs that your baby may or may not be coping well with labour before you make this decision.
Tachycardia
The other way that your team can tell if your baby is happy during labour is by evaluating the baby’s heartrate. If you have chosen to start your labour with intermittent monitoring, using a hand-held monitor, the presence of meconium in your baby’s fluid would be a reason to recommend continuous monitoring. Professionals often refer to the trace from continuous fetal heart rate monitoring as a CTG, which stands for cardiotocograph. There are a few things we look for in a CTG trace to tell if your baby is coping well. But one of the things we consider important in a breech birth is called the baseline.
The baseline of your baby’s heart rate is another way of saying the average heart rate. Normally, this ranges from about 120 bpm to 160 bpm in labour. Just like ours, your baby’s heart rate fluctuates in labour. When your baby moves, the heart rate on a CTG often goes up, or accelerates, just like yours would if you are climbing a flight of stairs. We consider this a really positive sign of your baby’s well-being.
But if your baby’s heart rate climbs up to over 160 bpm and stays in that range, rather than settling back down to where it was when we first listened in during your labour, that is another sign that your baby is finding things a bit stressful. We call an average heartrate over 160 bpm a fetal tachycardia. Tachycardia is always a sign that your baby is compensating for something. This is likely to be either an infection or hypoxia, which means oxygen deprivation. Your baby can’t breathe faster, so instead their heart beats faster to circulate the available oxygen. Again, most babies cope well with this for limited amounts of time. That’s what they are designed to do.
However, if your baby is experiencing more than thirty minutes of tachycardia that does not settle in the first stage of labour, the team will offer you a caesarean birth. If this is the only concern in your labour, for example the fluid around your baby is draining beautifully clear, and we see lots of accelerations on the CTG as well, your care providers may be comfortable with observing for a bit longer. This is especially likely if your labour appears to be progressing very quickly or if your baby is near to being born.
Meconium AND tachycardia
But when these occur together – tachycardia AND meconium in labour – your OptiBreech team will change from offering you a caesarean birth to advising one, especially if these occur in the first stage of labour. When BOTH tachycardia and meconium are present, they are both more likely to be associated with infection and inflammation.
When meconium is present in labour, in most cases, it has no consequence for the baby. But in 5% or 1:20 cases where we observe meconium in labour, the baby inhales meconium during the birth process and shows signs of what we call meconium aspiration syndrome after the birth. Meconium aspiration is more likely if the baby becomes severely stressed due to low oxygen levels and tries to take a breath before they are born. They then inhale the meconium-stained fluid into their lungs. This can result in breathing problems and require admission to the neonatal intensive care unit. This is more likely if infection or inflammation processes are present. In about 1:5 cases of meconium aspiration, there can be long-term problems for the child associated with this, again more likely if infection and inflammation are present.
We also think this may be more likely in breech births because of the way these babies are born. In every breech birth, there will be a period just at the end when the baby’s cord is likely to be compressed. When deciding whether it is safe to start or continue pushing, your OptiBreech team will be evaluating how long this period is likely to be, and how well your baby is likely to cope with it. Again, most babies cope very well with this for a short period of time, especially if we keep their umbilical cord attached after birth. But if your baby is ALREADY compensating with a raised heart rate and THEN the birth is difficult at the end, your baby may be more likely to inhale meconium-stained fluid.
For many years, the primary strategy to reduce risk in vaginal breech births was to try to predict which babies would have problems based on ultrasound scans – this baby is a bit bigger than others, this baby has a foot tucked below his pelvis, etc. But unfortunately, this strategy is not very accurate. A lot of caesarean births are recommended when the babies are not at significantly different risk to other babies who do not have these characteristics before labour.
In OptiBreech care, our strategy is to respond to emergent risks in labour. This means we look out for signs during the course of labour itself that your baby may be one of the few who do not do well with a breech birth, and we give you this information as soon as possible. Prior to labour, we simply cannot predict which labours may be affected by meconium or tachycardia. The situation in which a baby inhales meconium during birth and has some long-term issues as a result only occurs in about 1:700 births; and that includes all births, not just breech.
Meconium is only present in about 1 in 7 births, so when we see this in the first stage of labour, we know that the risk is now about 1:100. We know that aspiration of the meconium will only occur in about 1:20 births where the meconium is present, but when tachycardia is also present, this risk is closer to about 1:5. If one or both of these appear close to the end of labour, it may not be as much of a risk because most of the meconium may be coming down and out rather than circulating in the amniotic fluid around the baby. Your team may judge that your labour is progressing quickly and the safest thing is still continue with a vaginal birth. But when both meconium and tachycardia appear in the first stage of labour, our clear recommendation is for the team to calmly take you down the corridor and assist you with a caesarean birth, with your consent, due to the 1:5 risk of meconium aspiration with potential long-term problems.
I hope this helps explain why we consider meconium and tachycardia signs of potential risk for your baby, especially when they occur together, and even more so when they are present early in labour. I want to reassure you, that most babies will be absolutely fine, even if meconium or tachycardia occur during labour. Most babies are very resilient, like their mothers.
But the premise of OptiBreech care is that we are always honest with you about any potential increased risks that we detect. And we ask our teams to always honour your wishes about what you want to do with that information. We feel confident to support more people to attempt a vaginal birth because together, the OptiBreech collaborative are developing new guidelines, based on what we see happening in our research, to help keep you and your baby as safe as possible.
References
Beligere, N., Rao, R., 2008. Neurodevelopmental outcome of infants with meconium aspiration syndrome: report of a study and literature review. J. Perinatol. 2008 283 28, S93–S101. https://doi.org/10.1038/jp.2008.154
Buhimschi, C.S., Abdel-Razeq, S., Cackovic, M., Pettker, C.M., Dulay, A.T., Bahtiyar, M.O., Zambrano, E., Martin, R., Norwitz, E.R., Bhandari, V., Buhimschi, I.A., 2008. Fetal heart rate monitoring patterns in women with amniotic fluid proteomic profiles indicative of inflammation. Am. J. Perinatol. 25, 359. https://doi.org/10.1055/S-2008-1078761
Lee, J., Romero, R., Lee, K.A., Kim, E.N., Korzeniewski, S.J., Chaemsaithong, P., Yoon, B.H., 2016. Meconium aspiration syndrome: a role for fetal systemic inflammation. Am. J. Obstet. Gynecol. 214, 366.e1-366.e9. https://doi.org/10.1016/J.AJOG.2015.10.009
Pereira, S., Chandraharan, E., 2017. Recognition of chronic hypoxia and pre-existing foetal injury on the cardiotocograph (CTG): Urgent need to think beyond the guidelines. Porto Biomed. J. 2, 124–129. https://doi.org/10.1016/J.PBJ.2017.01.004