Join the webinar using this Zoom link: https://us02web.zoom.us/j/85392795495?pwd=Z2NMelErWmZLb2xFOHhzR3ZSK0JlQT09

In this participatory research webinar, we will share the results of two of the OptiBreech qualitative research projects. We invite all stakeholders (participants, women & birthing people, clinicians, service leaders and policy makers) to reflect on our findings with us and shape the interpretations we will summarise in our papers’ discussions.
Work will be presented by Research Assistants Honor Vincent and Alice Hodder, along with our PPIE Lead, Sian Davies. Abstracts of the two papers are below. If you have contributed to the research (clinicians and research staff), you will receive a copy of our draft paper and an invitation to make comments and/or recommendations for revisions.
If you are a stakeholder, we invite you to share your views in the meeting chat, raise them when we open the meeting for discussion or send them directly to a member of the research team.

For all sites that have expressed an interest in our planned stepped wedge trial of OptiBreech collaborative care: please include your name and hospital in the webinar chat, and we will award one site selection point for every site that participates.
Barriers and facilitators for team implementation of OptiBreech collaborative care
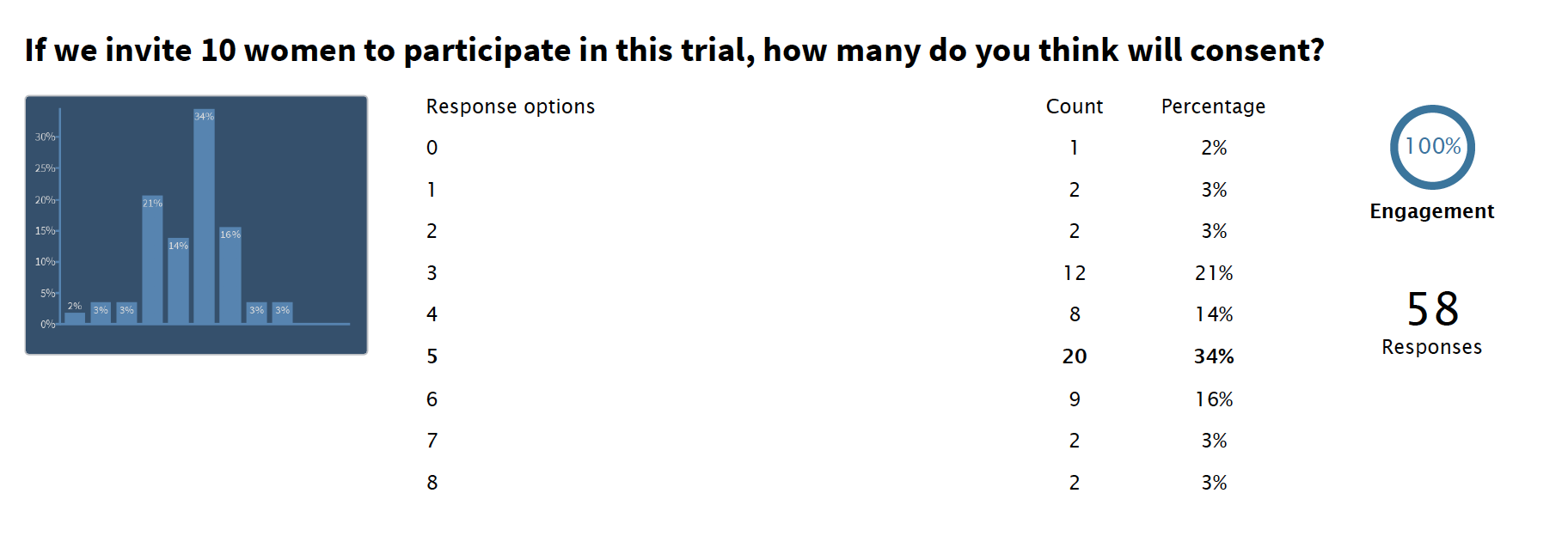
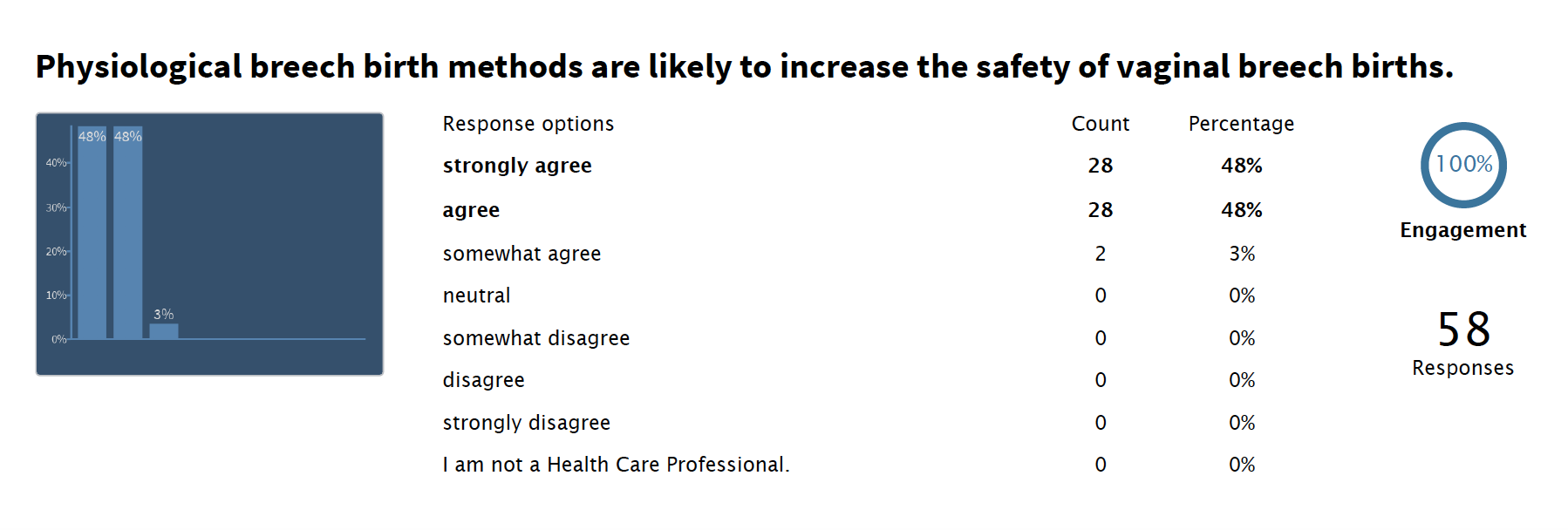
Introduction: Increased rates of caesarean section for breech presentation and lack of training have reduced professional experience and expertise in supporting vaginal breech birth. OptiBreech collaborative care is a care pathway that aims to enable maternal choice and improve training opportunities for maternity professionals, through dedicated clinics and intrapartum support. In feasibility work, barriers and facilitators to team implementation were observed by team members. This study seeks to describe these factors to optimise future implementation of OptiBreech collaborative care.
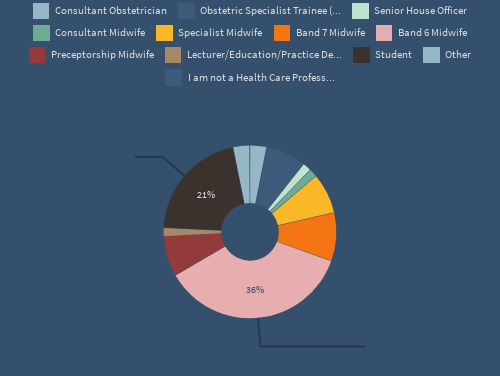
Methods: Semi-structured interviews were conducted with staff members at OptiBreech trial sites (17 midwives and 4 obstetricians, n=21), via video conferencing software. A Theoretical Domains Framework (TDF) was used to identify factors impacting team implementation. Themes identified in the TDF were refined in reflective discussion and grouped into key facilitators, key barriers, and dynamic factors (which span both barriers and facilitators). The interviews were then coded, analysed and interpreted according to the refined framework.
Results: The key facilitators were broadly categorised within skill development, beliefs about capabilities and social support from the wider multidisciplinary team. Key barrier categories were resources, social obstacles and fears about consequences. Dynamic factor categories were individual responsibility, training and practice.
Conclusions: While some factors affecting implementation were specific to the individuals and cultures of certain trusts, recommendations emerged from analysis that are more broadly applicable across multiple trusts. These should be considered going forward for future trust implementation in the next stage of clinical trials.
The OptiBreech Trial feasibility study: a qualitative inventory of the roles and responsibilities of breech specialist midwives
Background: The safety of vaginal breech birth (VBB) is associated with the skill and experience of professionals in attendance, but minimal training opportunities have led a to a lack of willingness to support these births. OptiBreech collaborative care is a pathway designed to support maternal choice and professional training, through dedicated breech clinics and intrapartum support. In feasibility work for the OptiBreech Trial, these were usually co-ordinated by a key midwife on the team, functioning as a specialist.
Objective: To describe the roles and tasks undertaken by breech specialists in the OptiBreech 1 study (NIHR300582).
Methods: Semi-structured interviews were conducted with OptiBreech team members (17 midwives and 4 obstetricians, n=21), via video conferencing software. Template analysis was used to code, analyse, and interpret data relating to the roles of the midwives delivering breech services. Tasks identified through initial coding were organised into five key themes in a template, following reflective discussion at weekly staff meetings. This template was then applied to all interviews to structure the analysis.
Results: Breech specialists as change agents emerged as important in multiple settings; each fulfilled similar roles to support their teams, whether this role was formally recognised or not. In this study, this role was most commonly described as fulfilled by midwives, but some obstetricians also functioned as specialists. We report an inventory of tasks performed by breech specialist midwives, organised into five themes: Care Planning, Clinical Care, Education and Training, Service Development, and Research.
Conclusions: Breech Specialists perform a consistent set of roles and responsibilities to co-ordinate care throughout the OptiBreech pathway. The inventory has been formally incorporated into the OptiBreech collaborative care intervention. This detailed description can also be used by employers and professional organisations who wish to formalise similar roles to meet consistent standards and improve care.
Keywords: breech birth; specialist midwife; intrapartum care; trial feasibility